Acne is often dismissed as a cosmetic concern or a problem of adolescence, yet for countless women it is a long-term, recurring condition deeply tied to hormonal health. Many women notice that their skin follows patterns; breaking out at certain points in the month, flaring alongside irregular periods, or changing dramatically after starting or stopping birth control. These patterns are not coincidental. They are reflections of the complex hormonal systems that regulate the female body.
Hormonal acne is not simply about having “too much oil” or using the wrong skincare products. It is the visible result of internal hormonal shifts, sensitivities, and imbalances. To understand why acne behaves the way it does, it is essential to understand how the menstrual cycle functions, how conditions such as Polycystic Ovary Syndrome (PCOS) alter hormone levels, and how hormonal contraceptives intervene in these processes.
This article explores these connections in depth, offering a clear and science-based explanation of why acne appears, worsens, or improves under different hormonal circumstances.
Hormonal Nature of Acne in Women
At its core, acne is an inflammatory condition of the pilosebaceous unit, which consists of the hair follicle and its attached oil gland. These oil glands are highly sensitive to hormones, particularly androgens such as testosterone and DHEA-S. While these hormones are often associated with men, they are naturally present and necessary in women as well. Problems arise not simply when androgen levels are high, but when the skin becomes overly responsive to them.
When androgen activity increases, oil glands produce more sebum. Excess sebum mixes with dead skin cells, clogging pores and creating an environment where acne-causing bacteria can thrive. This leads to inflammation, redness, tenderness, and in more severe cases, deep cystic lesions.
What makes acne in women particularly complex is that hormone levels are not static. They fluctuate daily, monthly, and across life stages. The menstrual cycle alone introduces dramatic hormonal shifts, and conditions like PCOS or the use of hormonal birth control further modify these internal signals.
Menstrual Cycle and Its Influence on Acne

For many women, acne follows a monthly rhythm. Breakouts may reliably appear in the days leading up to menstruation and improve shortly after the period begins. This phenomenon, often referred to as menstrual or cyclical acne, is directly tied to the hormonal changes that occur throughout the menstrual cycle.
The menstrual cycle is governed primarily by estrogen and progesterone, with androgens playing a supporting but influential role. During the first half of the cycle, estrogen gradually rises. Estrogen has a generally beneficial effect on the skin: it helps regulate oil production, supports skin barrier function, and promotes healing. As estrogen levels increase, many women notice their skin looks clearer, smoother, and more balanced.
Ovulation marks a brief hormonal peak. Around this time, there is also a temporary rise in testosterone. In some women, this has little visible effect; in others, it may trigger small breakouts, particularly if the skin is highly androgen-sensitive.
The most acne-prone phase of the cycle occurs after ovulation, during the luteal phase. Progesterone rises to prepare the body for a potential pregnancy, while estrogen levels gradually decline. Progesterone can cause the skin to swell slightly, narrowing pores and making them more prone to blockage. At the same time, the relative influence of androgens increases, even if their absolute levels do not dramatically rise. Oil production becomes heavier, pores clog more easily, and inflammation increases.
This is why many women experience acne in the week or two before their period. These breakouts often appear on the lower face; particularly the chin, jawline, and neck; and tend to be deeper, more tender, and slower to heal than typical surface pimples.
Once menstruation begins, estrogen and progesterone drop sharply. For many women, this hormonal reset allows inflammation to subside and breakouts to gradually improve.
When Acne Is More Than Cyclical: Understanding PCOS

While menstrual acne is common and usually predictable, some women experience acne that is persistent, severe, and resistant to typical treatments. In many cases, this points to an underlying hormonal condition, most notably Polycystic Ovary Syndrome.
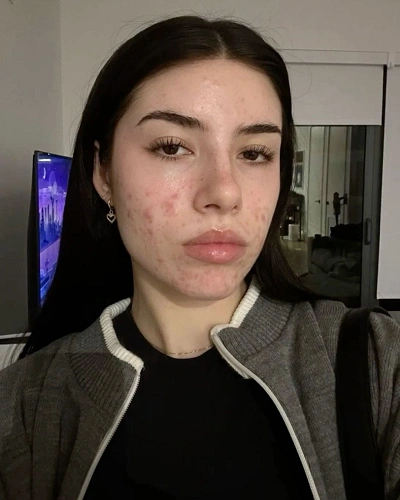
PCOS is a complex endocrine disorder that affects a significant portion of women of reproductive age. One of its defining features is chronically elevated androgen levels or increased sensitivity to androgens. Unlike the temporary hormonal shifts of a normal menstrual cycle, PCOS creates a sustained hormonal environment that continuously stimulates oil production.
In women with PCOS, acne is often more severe and long-lasting. It may persist throughout the entire month rather than appearing only before menstruation. Breakouts are frequently cystic, painful, and concentrated along the jawline, chin, neck, and sometimes the upper back and chest. Because the hormonal trigger is ongoing, the skin rarely gets a true “break,” which increases the risk of scarring and post-inflammatory pigmentation.
PCOS-related acne often occurs alongside other symptoms, including irregular or absent periods, difficulty ovulating, excessive facial or body hair, thinning scalp hair, and metabolic issues such as insulin resistance. Insulin resistance itself can worsen acne by increasing androgen production, creating a feedback loop that further aggravates the skin.
It is important to note that not all women with PCOS look the same or experience all symptoms. Some women have regular periods but elevated androgens; others struggle primarily with acne and hair changes. Acne alone does not diagnose PCOS, but when it is persistent and accompanied by other signs of hormonal imbalance, further medical evaluation is essential.
Role of Birth Control in Acne Development and Management

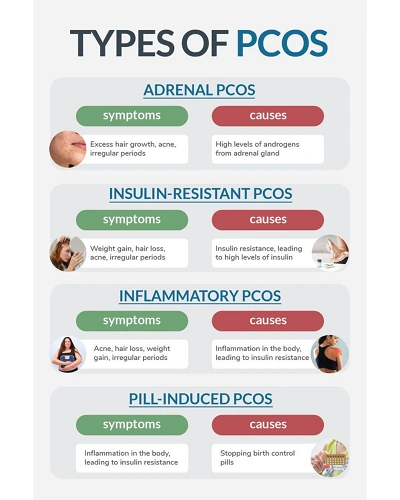
Hormonal birth control adds another layer of complexity to the relationship between hormones and acne. For some women, birth control is a powerful tool for clearing hormonal acne. For others, it becomes the trigger for breakouts that never existed before.
Combined hormonal contraceptives contain both estrogen and progestin. Estrogen in birth control helps reduce acne by lowering the amount of free testosterone in the bloodstream and decreasing oil gland activity. Certain formulations are specifically approved for acne treatment because they counteract androgen effects effectively.
However, not all progestins behave the same way. Some have androgen-like properties, meaning they can stimulate oil production rather than suppress it. In women who are already sensitive to hormonal changes, these formulations may worsen acne or cause new breakouts to appear.
Progestin-only methods, such as certain pills, injections, implants, and hormonal intrauterine devices, lack the balancing effect of estrogen. As a result, androgen activity may become more pronounced, leading to increased oil production and acne in some users.
Another common experience is acne after stopping birth control. While on hormonal contraception, natural hormone production is suppressed. When birth control is discontinued, the body must recalibrate. During this adjustment period, androgens may temporarily surge, oil glands may become overactive, and acne can flare; sometimes severely. This post-pill acne often appears months after stopping and can be confusing and distressing, particularly for women who never struggled with acne before using birth control.
10 Evidence Based Steps to Resolve Hormonal Acne

While hormonal acne can feel overwhelming, it is manageable with the right approach. The following steps address acne from the inside out, targeting the root hormonal drivers rather than just surface symptoms.
1. Track Your Cycle and Acne Patterns
Begin by observing when breakouts appear, how severe they are, and how long they last. Cycle-related acne often flares before menstruation, while persistent acne may suggest PCOS or hormonal imbalance. Pattern recognition is essential for choosing the right treatment strategy.
2. Support Hormonal Balance Through Nutrition
Blood sugar instability and insulin resistance can worsen androgen activity. Prioritizing balanced meals with adequate protein, fiber, and healthy fats helps regulate insulin and reduce hormonal acne triggers, especially in women with PCOS.
3. Reduce Chronic Inflammation
Hormonal acne is inflammatory by nature. Diets high in ultra-processed foods, refined sugars, and trans fats can worsen inflammation, while anti-inflammatory foods such as vegetables, omega-3 fats, and antioxidants support clearer skin.
4. Manage Stress and Cortisol Levels
Chronic stress increases cortisol, which can stimulate oil production and worsen hormonal imbalance. Stress management through sleep, movement, breathwork, or mindfulness is not optional; it is foundational for hormonal skin health.
5. Choose Skincare That Supports Hormonal Acne
Harsh, stripping products can damage the skin barrier and increase inflammation. Gentle cleansing, barrier-supportive moisturizers, and non-comedogenic formulations are essential. Hormonal acne requires consistency, not aggression.
6. Address Androgen Activity When Necessary
In cases of persistent or cystic acne, particularly with PCOS, medical treatments that reduce androgen effects may be required. This step is often crucial when topical treatments repeatedly fail.
7. Evaluate Birth Control Thoughtfully
If acne worsened after starting birth control, the formulation may not be right for your hormonal profile. If acne flared after stopping, the skin may need time and support during hormonal readjustment. Birth control decisions should consider skin health alongside reproductive goals.
8. Support Gut Health
The gut plays a significant role in hormone metabolism and inflammation. Poor gut health can impair estrogen clearance and worsen acne. A fiber-rich diet and digestive support can indirectly improve hormonal skin conditions.
9. Be Patient With Hormonal Healing
Hormonal acne does not resolve overnight. Because hormones operate on longer cycles, meaningful improvement often takes several months. Consistency is far more important than rapid changes or frequent product switching.
10. Seek Professional Guidance When Needed
If acne is painful, scarring, emotionally distressing, or accompanied by irregular periods or excess hair growth, professional evaluation is essential. Hormonal testing and individualized treatment plans can prevent years of unnecessary trial and error.
Emotional and Psychological Impact of Hormonal Acne

Hormonal acne is not just a physical condition; it carries a significant emotional burden. Breakouts often coincide with other hormonally driven symptoms such as mood swings, fatigue, bloating, and anxiety. For women dealing with PCOS or fertility concerns, acne can become a constant visual reminder of an internal struggle.
Because hormonal acne frequently affects the lower face, it is highly visible and difficult to conceal. Many women feel frustrated, embarrassed, or helpless when topical treatments fail and well-meaning advice focuses only on surface-level solutions.
It is crucial to recognize that hormonal acne is not caused by poor hygiene, laziness, or a lack of discipline. It is a medical and physiological issue that often requires medical understanding and long-term management.
Understanding Patterns as a Path to Healing
One of the most powerful tools in managing hormonal acne is awareness. Observing when acne appears, how long it lasts, where it forms, and how it responds to life changes can provide valuable insight into underlying hormonal patterns.
Acne that flares predictably before menstruation suggests sensitivity to normal hormonal fluctuations. Acne that is constant and severe may point toward conditions like PCOS or insulin resistance. Acne that begins or worsens after starting or stopping birth control often reflects the body’s response to hormonal suppression or withdrawal.
Recognizing these patterns allows women to seek appropriate care rather than endlessly cycling through ineffective treatments.
Final Thoughts
The connection between menstrual cycles, PCOS, birth control, and acne is intricate, deeply biological, and highly individual. Acne is often the skin’s way of signaling that something internally is shifting or out of balance.
By understanding how hormones influence the skin, women can replace self-blame with self-awareness and pursue solutions that address the root cause rather than just the symptoms. Hormonal acne is common, valid, and manageable, but it requires patience, education, and often professional guidance.
Your skin is not working against you; it is communicating with you. Learning to understand that message is the first step toward long-term healing and confidence.